INTRODUCTION
As many as one-third of patients seen in the primary
care setting may experience occasional difficulties in
sleeping, and 10 percent of those may have chronic
sleep problems. Although insomnia is rarely the
chief reason for an office visit, its detection can be
enhanced by incorporating sleep-related questions
into the general review of patient systems.
This document offers up-to-date information on
insomnia and highlights the key role of the primary
care physician in its recognition and management.
Behavioral treatments, such as relaxation therapy,
sleep restriction therapy, and stimulus control therapy,
are described in addition to pharmacological
treatments, such as hypnotics, antidepressants, and
other medications.
As many as one-third of patients seen in the primary
care setting may experience occasional difficulties in
sleeping, and 10 percent of those may have chronic
sleep problems. Although insomnia is rarely the
chief reason for an office visit, its detection can be
enhanced by incorporating sleep-related questions
into the general review of patient systems.
This document offers up-to-date information on
insomnia and highlights the key role of the primary
care physician in its recognition and management.
Behavioral treatments, such as relaxation therapy,
sleep restriction therapy, and stimulus control therapy,
are described in addition to pharmacological
treatments, such as hypnotics, antidepressants, and
other medications.
DEFINITION AND PREVALENCE
Insomnia is an experience of inadequate or poor
quality sleep characterized by one or more of the
following:
• difficulty falling asleep
• difficulty maintaining sleep
• waking up too early in the morning
• nonrefreshing sleep.
Insomnia also involves daytime consequences such as
• tiredness
• lack of energy
• difficulty concentrating
• irritability.
INSOMNIA: ASSESSMENT AND
MANAGEMENT IN PRIMARY CARE
Periods of sleep difficulty lasting between one
night and a few weeks are referred to as acute
insomnia. Chronic insomnia refers to sleep
difficulty at least three nights per week for one
month or more.
About 30 to 40 percent of adults indicate some
level of insomnia within any given year, and about
10 percent to 15 percent indicate that the insomnia
is chronic and/or severe.1
The prevalence of insomnia increases with age and
is more common in women.
TYPES OF INSOMNIA
Acute Insomnia
Acute insomnia is often caused by emotional or
physical discomfort. Some common examples
include significant life stress; acute illness; and
environmental disturbances such as noise, light, and
temperature.3 Sleeping at a time inconsistent with
the daily biological rhythm, such as occurs with jet
lag, also can cause acute insomnia.
Acute Insomnia
Acute insomnia is often caused by emotional or
physical discomfort. Some common examples
include significant life stress; acute illness; and
environmental disturbances such as noise, light, and
temperature.3 Sleeping at a time inconsistent with
the daily biological rhythm, such as occurs with jet
lag, also can cause acute insomnia.
Chronic Insomnia
Chronic insomnia can be caused by many different
factors acting singly or in combination, and often
occurs in conjunction with other health problems.
In other cases sleep disturbance is the major or sole
complaint, and involves abnormal sleep-wake
regulation or physiology during sleep.
Insomnia associated with psychiatric, medical,
and neurological disorders. Although psychiatric
disorders are a common source of chronic insomnia,
they account for less than 50 percent of cases.
n delayed sleep phase syndrome
— difficulty falling asleep
at the desired time
— difficulty waking at the desired time
n advanced sleep phase syndrome
— difficulty staying awake
in the evening
— waking too early
n shift worker
— difficulty getting enough sleep during
available sleep times
Mood and anxiety disorders are the most common
psychiatric diagnoses associated with insomnia.
Chronic insomnia can be caused by many different
factors acting singly or in combination, and often
occurs in conjunction with other health problems.
In other cases sleep disturbance is the major or sole
complaint, and involves abnormal sleep-wake
regulation or physiology during sleep.
Insomnia associated with psychiatric, medical,
and neurological disorders. Although psychiatric
disorders are a common source of chronic insomnia,
they account for less than 50 percent of cases.
n delayed sleep phase syndrome
— difficulty falling asleep
at the desired time
— difficulty waking at the desired time
n advanced sleep phase syndrome
— difficulty staying awake
in the evening
— waking too early
n shift worker
— difficulty getting enough sleep during
available sleep times
Mood and anxiety disorders are the most common
psychiatric diagnoses associated with insomnia.
Insomnia can also be associated with a wide variety
of medical and neurological disorders. Factors
that cause problems throughout the day such as
pain, immobility, difficulty breathing, dementia,
and hormonal changes associated with pregnancy,
perimenopause, and menopause can also cause
insomnia. Many medical disorders worsen at night,
either from sleep per se, circadian influence (e.g.,
asthma), or recumbency (e.g., gastroesophageal
reflux).
of medical and neurological disorders. Factors
that cause problems throughout the day such as
pain, immobility, difficulty breathing, dementia,
and hormonal changes associated with pregnancy,
perimenopause, and menopause can also cause
insomnia. Many medical disorders worsen at night,
either from sleep per se, circadian influence (e.g.,
asthma), or recumbency (e.g., gastroesophageal
reflux).
Insomnia associated with medication and substance
use. A variety of prescription drugs, nonprescription
drugs, and drugs of abuse can lead to increased wakefulness
and poor-quality sleep. The likelihood of
any given drug contributing to insomnia is unpredictable
and may be related to dose, lipophilicity,
individual differences, and other factors. Some drugs
commonly related to insomnia are stimulating antidepressants,
steroids, decongestants, beta blockers,
caffeine, alcohol, nicotine, and recreational drugs.
Insomnia associated with specific sleep disorders.
Insomnia can be associated with specific sleep
disorders, including restless legs syndrome (RLS),
periodic limb movement disorder (PLMD), sleep
apnea, and circadian rhythm sleep disorders.
Restless Legs Syndrome is characterized by
unpleasant sensations in the legs or feet temporarily
relieved by moving the limbs. Symptoms increase
in the evening hours, especially when a person is
lying down and remaining still. The dysesthesias
cause difficulty falling asleep and are often accompanied
by periodic limb movements.
Periodic Limb Movement Disorder is characterized by
bilateral repeated, rhythmic, small-amplitude jerking
or twitching movements in the lower extremities, and
less frequently in the arms. These movements occur
every 20 to 90 seconds and can lead to arousals,
which are usually not perceived by the patient.
Rather, there is a report of nonrefreshing sleep.
Obstructive sleep apnea is most commonly associated
with snoring, daytime sleepiness, and obesity, but
occasionally can cause insomnia.
Circadian rhythm sleep disorders are characterized
by an inability to sleep because of a mismatch
between the circadian sleep rhythm and the desired
or required sleep schedule. Examples are given in
the box above.
by an inability to sleep because of a mismatch
between the circadian sleep rhythm and the desired
or required sleep schedule. Examples are given in
the box above.
Primary Insomnia. When other causes of insomnia
are ruled out or treated, remaining difficulty with
sleep may be classified as primary insomnia.
Factors such as chronic stress, hyperarousal, poor
sleep hygiene, and behavioral conditioning may
contribute to primary insomnia.
S E L E C T E D C I R C A D I A N R H Y T H M S L E E P D I S O R D E R S
CONSEQUENCES
The primary consequences of acute insomnia are
sleepiness, negative mood, and impairment of performance.
The severity of these consequences is related
to the amount of sleep lost on one or more nights.
Patients with chronic insomnia frequently complain of
fatigue, mood changes (e.g., depression, irritability),
difficulty concentrating, and impaired daytime functioning.
Because insomnia has a variety of causes,
the consequences may not be uniform. For example,
when objectively assessed, the level of daytime
sleepiness may be elevated with periodic limb
movement disorder and rheumatoid arthritis,14 but
not in primary insomnia.
CONSEQUENCES
The primary consequences of acute insomnia are
sleepiness, negative mood, and impairment of performance.
The severity of these consequences is related
to the amount of sleep lost on one or more nights.
Patients with chronic insomnia frequently complain of
fatigue, mood changes (e.g., depression, irritability),
difficulty concentrating, and impaired daytime functioning.
Because insomnia has a variety of causes,
the consequences may not be uniform. For example,
when objectively assessed, the level of daytime
sleepiness may be elevated with periodic limb
movement disorder and rheumatoid arthritis,14 but
not in primary insomnia.
Insomnia appears to contribute to increased rates of
absenteeism,16 health care utilization, and social
disability.
absenteeism,16 health care utilization, and social
disability.
RECOGNITION AND ASSESSMENT
A brief sleep history incorporated into the routine
review of systems can be helpful in detecting
insomnia. Direct inquiry is important because more
than half of the people who believe that they have
chronic insomnia have never discussed their problems
with a physician. Examples of appropriate questions
are shown in the box below. It is helpful for the
patient to keep a 1- to 2-week sleep diary. Sleep
diaries usually record bedtime, total sleep time, time
to sleep onset, number of awakenings, use of sleep
n How has the patient been sleeping recently?
A brief sleep history incorporated into the routine
review of systems can be helpful in detecting
insomnia. Direct inquiry is important because more
than half of the people who believe that they have
chronic insomnia have never discussed their problems
with a physician. Examples of appropriate questions
are shown in the box below. It is helpful for the
patient to keep a 1- to 2-week sleep diary. Sleep
diaries usually record bedtime, total sleep time, time
to sleep onset, number of awakenings, use of sleep
n How has the patient been sleeping recently?
Suggested Questions Following a Complaint of Insomnia
n When did the problem begin? (to determine acute vs. chronic.)
n Does the patient have a psychiatric or medical condition that may cause insomnia?
n Is the sleep environment conducive to sleep (relative to noise, interruptions, temperature, light)?
n Does the patient report “creeping, crawling, or uncomfortable feelings” in the legs relieved by moving them?
(Relates to restless legs syndrome.)
n Does the bed partner report that the patient’s legs or arms jerk during sleep?
(Relates to periodic limb movements in sleep.)
n Does the patient snore loudly, gasp, choke, or stop breathing during sleep? (Relates to obstructive sleep apnea.)
n Is the patient a shift worker? What are the work hours? Is the patient an adolescent? (Relates to circadian sleep
disorders/sleep deprivation.)
n What are the bedtimes and rise times on weekdays and weekends? (Relates to poor sleep hygiene.)
n Does the patient use caffeine, tobacco or alcohol? Does the patient take over-the-counter or prescription medications
(such as stimulating antidepressants, steroids, decongestants, beta blockers)? (Relates to substance-induced
insomnia.)
Signs of Sleepiness
n What daytime consequences does the patient report?
n Does the patient report dozing off or difficulty staying awake during routine tasks, especially while driving
S L E E P / W A K E P R O F I L E
medications, time out of bed in the morning, and a
rating of subjective quality of sleep and daytime
symptoms. The sleep diary provides a night-tonight
account of the patient’s sleep schedule and
perception of his or her sleep. Moreover, it may
serve as a baseline for assessment of treatment
effects. Completing the diary each morning, and
using estimates rather than exact times, should
minimize the likelihood that the process itself will
be disruptive to sleep. See table 1 for a sample
sleep diary.
medications, time out of bed in the morning, and a
rating of subjective quality of sleep and daytime
symptoms. The sleep diary provides a night-tonight
account of the patient’s sleep schedule and
perception of his or her sleep. Moreover, it may
serve as a baseline for assessment of treatment
effects. Completing the diary each morning, and
using estimates rather than exact times, should
minimize the likelihood that the process itself will
be disruptive to sleep. See table 1 for a sample
sleep diary.
Assessment should include questions that address
both sleep and daytime functioning, mainly because
sleep needs vary markedly from person to person.
One patient sleeping 6 hours may feel totally unrefreshed,
while another one may be sleeping 6 hours
but have no complaints during the day.
Although the ability to maintain sleep decreases
with age, the need for sleep does not change significantly.
A complaint of simply not sleeping “a full
8 hours” but otherwise having restorative sleep is
within the bounds of normal behavior, and reassurance
may be all that is needed. However, a complaint
of severe insomnia or excessive daytime
sleepiness should prompt an evaluation, regardless
of the patient’s age.
MANAGEMENT
Introduction
Often the cause of acute insomnia (no one episode
lasts longer than several weeks) is related to a
single specific event. The need for treatment is
usually determined by the severity of the daytime
sequelae, the duration of the episode, and the
degree to which episodes become predictable.
Even brief episodes of acute insomnia may warrant
treatment because individuals who are typically
good sleepers can and do become significantly
sleepy after loss of just a few hours of sleep on one
or more nights. Also, there is a possibility that
untreated acute insomnia may develop into a
chronic, learned insomnia.
Introduction
Often the cause of acute insomnia (no one episode
lasts longer than several weeks) is related to a
single specific event. The need for treatment is
usually determined by the severity of the daytime
sequelae, the duration of the episode, and the
degree to which episodes become predictable.
Even brief episodes of acute insomnia may warrant
treatment because individuals who are typically
good sleepers can and do become significantly
sleepy after loss of just a few hours of sleep on one
or more nights. Also, there is a possibility that
untreated acute insomnia may develop into a
chronic, learned insomnia.
n Wake up at the same time of day.
n Discontinue caffeine 4 to 6 hours before bedtime,
and minimize total daily use. Caffeine is a
stimulant and may disrupt sleep.
n Avoid nicotine, especially near bedtime and
upon night awakenings; it is also a stimulant.
n Avoid the use of alcohol in the late evening to
facilitate sleep onset; alcohol can cause awakenings
later in the night.
n Avoid heavy meals too close to bedtime, as this
may interfere with sleep. A light snack may be
sleep-inducing.
n Regular exercise in the late afternoon may deepen
sleep; vigorous exercise within 3 to 4 hours
of bedtime may interfere with sleep.
n Minimize noise, light, and excessive temperature
during the sleep period.
n Move the alarm clock away from the bed if it is
a source of distraction.
G E N E R A L S L E E P H Y G I E N E M E A S U R E S
Sleep hygiene measures may help promote sleep in all people. Sleep hygiene measures involve health practices and
environmental influences relating to sleep.
Date Monday,
4/10
Bed Time (of previous night) 10:45 p.m.
Rise Time 7: 00 a.m.
Estimated time to fall 30
asleep (previous night) minutes
Estimated # of awakenings & 5 times
total time awake (previous night) 2 hours
Estimated amount of sleep 4 hours
obtained (during previous night)
Naps 3:30 p.m.
(Time & Duration) 45 minutes
Alcoholic Drinks 1 drink @ 8:00 p.m.
(Number & Time) 2 drinks @ 9:00 p.m.
List stresses Flat tire
experienced today Argued w/son
Rate how you felt today
1 - Very tired/sleepy
2 - Somewhat tired/sleepy 2
3 - Fairly alert
4 - Wide awake
Irritability
1=Not at all / 5=very 5=very
Medications
Complete in PM Complete in AM
When the insomnia persists beyond a night or two,
or becomes predictable, treatment should be
considered. Pharmacological treatment usually
predominates—especially the use of short-acting
hypnotics. Adjunctive sleep hygiene measures
may also be useful. The goal
of treatment is to improve the patient’s sleep, but
it may not be possible to achieve normal sleep
every night.
Chronic insomnia is often a significant therapeutic
challenge. Since chronic insomnia is often
multifactorial in etiology, multiple treatment
modalities may be needed for any one patient. If
an underlying medical or psychiatric condition is
identified, this condition should be treated first. In
some patients, the mechanisms that maintain the
insomnia are more important than precipitating
factors.
If the complaint of chronic insomnia appears to be
primary or persists after treatment of an underlying
condition, two general treatment approaches are
available—behavioral and pharmacological. Usually
pharmacological treatment provides rapid symptom
relief, but long-term treatment is unstudied.
Behavioral approaches take a few weeks to improve
sleep but continue to provide relief after training
sessions have been completed. Behavioral Treatment
Behavioral interventions seek to change maladaptive
sleep habits, reduce autonomic arousal, and
alter dysfunctional beliefs and attitudes, which are
presumed to maintain insomnia. These therapies
have been shown to produce reliable and durable
improvements for patients with chronic primary
insomnia.
At times, the various behavioral
treatments are compatible with each other and
can be combined, although it is not clear whether
increased therapeutic benefit results.
Relaxation Therapy. Relaxation therapy is based on
observations that insomnia patients often display
high levels of physiologic, cognitive, and/or emotional
arousal, both at night and during the daytime.
treatments are compatible with each other and
can be combined, although it is not clear whether
increased therapeutic benefit results.
Relaxation Therapy. Relaxation therapy is based on
observations that insomnia patients often display
high levels of physiologic, cognitive, and/or emotional
arousal, both at night and during the daytime.
There are several relaxation methods
although none has been shown to be more efficacious
than the others. Progressive muscle relaxation,
autogenic training, and EMG biofeedback
seek to reduce somatic arousal (e.g., muscle tension),
whereas attention-focusing procedures such
as imagery training or meditation are intended at
lowering presleep cognitive arousal (e.g., intrusive
thoughts, racing mind). Abdominal breathing is
often a component of various relaxation techniques,
or it may be used alone. Relaxation therapy
is useful for both sleep onset and maintenance
insomnia. All these techniques require regular
practice with a trained professional over a period
of several weeks.
Sleep Restriction Therapy. Poor sleepers often
increase their time in bed in a misguided effort to
provide more opportunity for sleep, a strategy that
is more likely to result in fragmented and poorquality
sleep. Sleep restriction therapy23 consists
of curtailing the amount of time spent in bed to
increase the percentage of time asleep. This
improves the patient’s sleep efficiency (time
asleep/time in bed). For example, a person who
reports staying in bed for 8 hours but sleeping an
average of 5 hours per night would initially be told
to decrease the time in bed to 5 hours. The allowable
time in bed per night is increased 15 to 30
minutes as sleep efficiency improves. Adjustments
are made over the weeks until an optimal sleep
duration is achieved.
Typically, it is best to alter
bedtime and keep the rise time constant in order to
maintain a regular sleep-wake rhythm. By creating
a mild state of sleep deprivation, this therapy promotes
more rapid sleep onset and more efficient
sleep. To minimize daytime sleepiness, time in
bed should not be reduced to less than 5 hours per
night. Sleep restriction therapy is modified in
older adults by allowing a short afternoon nap.
bedtime and keep the rise time constant in order to
maintain a regular sleep-wake rhythm. By creating
a mild state of sleep deprivation, this therapy promotes
more rapid sleep onset and more efficient
sleep. To minimize daytime sleepiness, time in
bed should not be reduced to less than 5 hours per
night. Sleep restriction therapy is modified in
older adults by allowing a short afternoon nap.
Stimulus Control Therapy.
Stimulus control therapy is based on the premise that insomnia is a conditioned
response to temporal (bedtime) and environmental
(bed/bedroom) cues usually associated with
sleep. The main objective of stimulus control therapy
is to reassociate the bed and bedroom with
rapid sleep onset. Stimulus control instructions
involve (a) going to bed only when sleepy; (b)
using the bed and bedroom only for sleep; (c) getting
out of bed and going into another room when
unable to fall asleep or return to sleep easily, and
returning to bed only when sleepy again; (d) maintaining
a regular rise time in the morning regardless
of sleep duration the previous night, and (e) avoiding
daytime napping.
response to temporal (bedtime) and environmental
(bed/bedroom) cues usually associated with
sleep. The main objective of stimulus control therapy
is to reassociate the bed and bedroom with
rapid sleep onset. Stimulus control instructions
involve (a) going to bed only when sleepy; (b)
using the bed and bedroom only for sleep; (c) getting
out of bed and going into another room when
unable to fall asleep or return to sleep easily, and
returning to bed only when sleepy again; (d) maintaining
a regular rise time in the morning regardless
of sleep duration the previous night, and (e) avoiding
daytime napping.
Clinical trials have documented
the efficacy of stimulus control therapy for both
sleep onset and sleep-maintenance insomnia. Cognitive Therapy.
the efficacy of stimulus control therapy for both
sleep onset and sleep-maintenance insomnia. Cognitive Therapy.
Cognitive therapy involves identifying
dysfunctional beliefs and attitudes about
sleep and replacing them with more adaptive substitutes.
For example, patients who believe that
sleeping 8 hours per night is an absolute necessity
to function during the day are asked to question the
evidence and their own experience to see if this is
true for them. Those who are convinced that
insomnia is destroying their ability to enjoy life are
encouraged to develop more adaptive coping skills
and to cease viewing themselves as victims.
dysfunctional beliefs and attitudes about
sleep and replacing them with more adaptive substitutes.
For example, patients who believe that
sleeping 8 hours per night is an absolute necessity
to function during the day are asked to question the
evidence and their own experience to see if this is
true for them. Those who are convinced that
insomnia is destroying their ability to enjoy life are
encouraged to develop more adaptive coping skills
and to cease viewing themselves as victims.
These attitudinal changes often help to minimize anticipatory
anxiety and arousal that interfere with sleep.
Pharmacological Treatment
Hypnotic Medications. The primary indication for
hypnotic medication is the short-term management
of insomnia—either as the sole treatment modality
or as adjunctive therapy until the underlying problem
is controlled. The most common type of medications
used to promote sleep are the benzodiazepine
receptor agonists. These compounds have
all been shown to be effective in inducing, maintaining,
and consolidating sleep as compared with a
placebo.
anxiety and arousal that interfere with sleep.
Pharmacological Treatment
Hypnotic Medications. The primary indication for
hypnotic medication is the short-term management
of insomnia—either as the sole treatment modality
or as adjunctive therapy until the underlying problem
is controlled. The most common type of medications
used to promote sleep are the benzodiazepine
receptor agonists. These compounds have
all been shown to be effective in inducing, maintaining,
and consolidating sleep as compared with a
placebo.
Patients report significant relief of both
nighttime and daytime symptoms.There are
small differences between compounds in their ability
to induce and maintain sleep based on rate of
absorption and elimination. The most common
side effect of these drugs is anterograde amnesia
and, for long-acting drugs, residual daytime drowsiness.
Currently an estimated 10 to 15 percent of
hypnotic users take them regularly for more than 1
year, although there are little safety or efficacy
data to guide their use beyond 2 to 3 months.
While selected patients may benefit from chronic
use, there are no clear indications of which patients
might benefit from chronic therapy.
nighttime and daytime symptoms.There are
small differences between compounds in their ability
to induce and maintain sleep based on rate of
absorption and elimination. The most common
side effect of these drugs is anterograde amnesia
and, for long-acting drugs, residual daytime drowsiness.
Currently an estimated 10 to 15 percent of
hypnotic users take them regularly for more than 1
year, although there are little safety or efficacy
data to guide their use beyond 2 to 3 months.
While selected patients may benefit from chronic
use, there are no clear indications of which patients
might benefit from chronic therapy.
Dose, pharmacokinetic properties (absorption rate,
distribution, elimination half-life), and risk-benefit
ratio are the key factors in selecting the most
appropriate medication. Dose is the single best
predictor of the frequency of side effects reported
with these medications. It impacts both the peak
amount of a drug in the body as well as the duration
of action of the medication. Once an effective
dose is established, increasing the dose rarely leads
to increased efficacy but does reliably predict an
increase in the frequency of side effects.
Elimination half-life varies considerably among
hypnotics and is the best predictor of next-day
residual effects.
For patients who need to be alert
because of occupational or societal demands, shortacting
medications are preferred. However, patients
with insomnia and high levels of daytime anxiety
may benefit more from long-acting medications. It
is important to remember that the volume of distribution
and rate of metabolism for most of these
medications slow with age. This leads to higher
drug concentrations and a longer duration of action.
Hypnotic medications are contraindicated in pregnant
women, patients with untreated obstructive
sleep apnea, patients with a history of substance
abuse, and patients who might need to awaken
and function during their normal sleep period.
because of occupational or societal demands, shortacting
medications are preferred. However, patients
with insomnia and high levels of daytime anxiety
may benefit more from long-acting medications. It
is important to remember that the volume of distribution
and rate of metabolism for most of these
medications slow with age. This leads to higher
drug concentrations and a longer duration of action.
Hypnotic medications are contraindicated in pregnant
women, patients with untreated obstructive
sleep apnea, patients with a history of substance
abuse, and patients who might need to awaken
and function during their normal sleep period.
Finally, patients with hepatic, renal, or pulmonary
disease need to be monitored more carefully than
otherwise healthy insomniacs.
Antidepressants. It is very common for sedating
antidepressants to be prescribed for insomnia, often
in low dose, but there is little scientific evidence to
support the efficacy or safety of this approach in
most types of insomnia.
When prescribed to patients with major depression, sedating antidepressants
improve subjective and objective measures
of insomnia, and sleep symptoms often
improve more quickly than other symptoms of
depression.
When administered concurrently with
“alerting” antidepressants, low doses of sedating
antidepressants such as trazodone again improve
insomnia.However, in nondepressed individuals
there are minimal data upon which to recommend
use of antidepressants.
improve subjective and objective measures
of insomnia, and sleep symptoms often
improve more quickly than other symptoms of
depression.
When administered concurrently with
“alerting” antidepressants, low doses of sedating
antidepressants such as trazodone again improve
insomnia.However, in nondepressed individuals
there are minimal data upon which to recommend
use of antidepressants.
Antidepressants have a range of adverse effects
including anticholinergic effects, cardiac toxicity,
orthostatic hypotension, and sexual dysfunction
(selective serotonin reuptake inhibitors [SSRIs]).
Tricyclic antidepressants and SSRIs can exacerbate
RLS and PLMD in some individuals. The lethal
dose/effective dose ratio for tricyclics is worse than
for benzodiazepines.
including anticholinergic effects, cardiac toxicity,
orthostatic hypotension, and sexual dysfunction
(selective serotonin reuptake inhibitors [SSRIs]).
Tricyclic antidepressants and SSRIs can exacerbate
RLS and PLMD in some individuals. The lethal
dose/effective dose ratio for tricyclics is worse than
for benzodiazepines.
With little scientific evidence supporting the
efficacy and safety of antidepressants in insomnia,
the clearest indications are for patients with insomnia
associated with psychiatric disorders or a previous
history of substance abuse.
Antihistamines. Drugs that antagonize central histamine-
1 receptors have sedative effects. The most
common antihistamines used for insomnia are
diphenhydramine and hydroxyzine; most over-thecounter
sleep aids include an antihistamine. Few
recent studies assess the efficacy of antihistamines
for treating insomnia, but older studies demonstrate
subjective and objective improvements during shortterm
treatment. The long-term efficacy of antihistamines
for insomnia has not been demonstrated.
Adverse effects associated with antihistamines
include daytime sedation, cognitive impairments, and
anticholinergic effects. Tolerance and discontinuation
effects have been noted
Melatonin. Melatonin has several physiological
actions, including a phase-shifting effect on circadian
rhythms, increased sleepiness when administered
during daytime hours, and vasoconstriction. Its
mechanisms of action are unknown but may
involve interaction with melatonin receptors in the
suprachiasmatic nucleus. The role of melatonin in
treating any sleep-related disorder remains to be
defined.34 Clinical studies in patients with insomnia
have provided inconsistent results.
Other Drugs. Barbiturates and a number of older
non-benzodiazepine, non-barbiturate drugs such as
chloral hydrate, methyprylon, and meprobamate
are still available. These drugs are not recommended
for treatment of insomnia because of their narrow
therapeutic ratio, rapid development of tolerance,
systemic toxicity, potential for abuse, and possibility
of severe clinical complications on withdrawal.
A variety of herbal preparations (e.g., valerian
root, herbal teas), nutritional substances (e.g.,
L-tryptophan), and over-the-counter drugs are also
promoted for the treatment of insomnia. In general,
there is little scientific evidence for the efficacy
or safety of these products.
Traditional Chinese Medicine Views on Insomnia....
Insomnia is inadequate or poor-quality sleep due to one or more of following:
| difficulty falling asleep; | |
| shallow sleep or dream-disturbed sleep; | |
| waking up frequently during the night and difficulty returning to sleep; | |
| waking up too early in the morning; | |
| inability to sleep at all during the night. |
Among the correlations between the organs and mental functions; the heart is the most important as it houses the shen; the kidney governs the storage of jing and promotes it transforming into marrow in the brain; the spleen acts as the nourishing source of mental activity; the liver governs the flow and discharge actions that regulates mental activity directly; and the gallbladder governs some important aspects of mental functioning such as decision making. Insomnia may follow when these organs are in disharmony.
Generally, the following contribute to the development of insomnia:
1. Mental distress
Anxiety and anger impair the normal functions of the liver, resulting in liver-qi stagnation. The stagnated qi transforms into fire evils and tends to attack the shen (spirit). Emotional extremes also induce the heart to form fire evils. When the spirit becomes irritable, insomnia will result. Furthermore, TCM believes that fear or other emotional stress gradually makes the heart and gallbladder weaken leading to wandering of the spirit and poor sleep. Excessive thinking or mentally exhaustion damages the heart and spleen, consumes the fundamental substances, resulting in an inadequate nutrient supply for the spirit, and thus in the development of insomnia.
2. Improper diet
Overeating, eating too much hot and spicy food, dried/fried foods or too heavy/greasy food can damage the spleen and stomach systems, which leads to slow transformation and transportation processes within the body. The retention of food will bring about phlegm accumulation and the development of heat evils which travel upwards to induce insomnia.
3. Physical weakness
Constitutional weakness, aging or major illness will all bring about kidney damage. Once there is disruption between heart and kidney, pathological conditions will occur. The depleted kidney-yin will not be able to nourish the heart, leading to hyperactivity of the heart and mental impairment. In addition, major blood loss or inadequate blood production will lead to heart weakness, which leads to uneasiness of the shen (spirit). If a weak and timid person is shocked by a sudden event, for example, their heart-qi will be greatly disturbed, resulting in dysfunction of the shen (spirit) and thus sleeping difficulties.
4. Imbalance between work and rest
TCM believes that overwork consumes excessive fundamental substances, while a too much leisure causes dysfunction of the spleen which leads to poor transformation and transportation from that organ. In either situation, the body's supply of essence, blood and other fundamental substances cannot maintain a stable shen (spirit), so sleep problems are likely to occur.
Generally, insomnia can be induced by many factors, mostly associated with mood and mental stress, diet, blood and qi deficiencies. These cause internal disturbances, non-smooth circulations and an imbalance of yin and yang. The main lesion is in the heart, and may also accompany spleen, kidney, liver, gallbladder and stomach disharmonies. Clinically, physicians classify insomnia into two major types:
| Deficient type: the shen (spirit) is undernourished, such as having insufficient blood or qi. | |
| Excess type: the shen (spirit) is irritated by pathogens, such as phlegm, fire and dampness as well as blood stasis. |
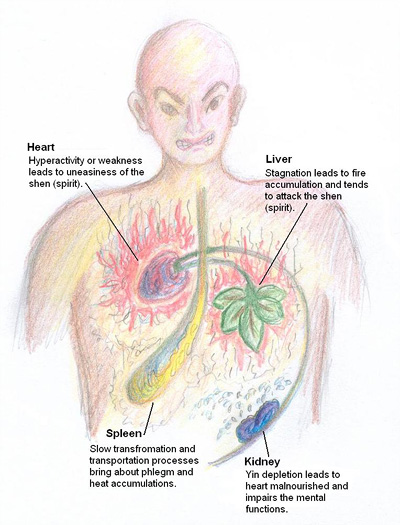 |
How traditional Chinese medicine views the development of insomnia
|
CONCLUSION
Sleep disturbance is a reliable predictor of psychological
and/or physical ill health. Thus a report of
disturbed sleep signals the need for further evaluation.
Physicians should inquire about sleep during
periodic patient assessments. Insomnia is often
associated with psychiatric or medical illness,
sometimes as the primary or first symptom of a
problem. Effective treatments for insomnia are
available. For some patients, improvement in sleep
leads to an improved quality of life.
Additional Sources and Reference Links
http://en.wikipedia.org/wiki/Insomnia
http://www.psychosomaticmedicine.org/content/62/4/483.full
http://www.primarypsychiatry.com/aspx/articledetail.aspx?articleid=1102
Hirshkowitz, Max (2004). "Chapter 10, Neuropsychiatric Aspects of Sleep and Sleep Disorders (pp 315-340)". In Stuart C. Yudofsky and Robert E. Hales, editors (Google Books preview includes entire chapter 10). Essentials of neuropsychiatry and clinical neurosciences (4 ed.). Arlington, Virginia, USA: American Psychiatric Publishing. ISBN 9781585620050. Retrieved 2009-12-06. "...insomnia is a symptom. It is neither a disease nor a specific condition. (from p. 322)"
^ Morin, Charles M. (2000). "The Nature of Insomnia and the Need to Refine Our Diagnostic Criteria" (Editorial). Psychosomatic Medicine 62 (4): 62:483–485. PMID 10949092. Retrieved 2010-01-07.
Diagnostic and Statistical Manual of Mental DIsorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
National Institutes of Health. National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005. Sleep. 2005;28(9):1049-1057.
International Classification of Sleep Disorders. Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
Sleep Disorders. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text revision. Washington, D.C.; American Psychiatric Association. 2000:551-607.
Kupfer DJ, Foster FG, Reich L, Thompson SK, Weiss B. EEG sleep changes as predictors in depression. Am J Psychiatry. 1976;133(6):622-626.
http://en.wikipedia.org/wiki/Insomnia
http://www.psychosomaticmedicine.org/content/62/4/483.full
http://www.primarypsychiatry.com/aspx/articledetail.aspx?articleid=1102
Hirshkowitz, Max (2004). "Chapter 10, Neuropsychiatric Aspects of Sleep and Sleep Disorders (pp 315-340)". In Stuart C. Yudofsky and Robert E. Hales, editors (Google Books preview includes entire chapter 10). Essentials of neuropsychiatry and clinical neurosciences (4 ed.). Arlington, Virginia, USA: American Psychiatric Publishing. ISBN 9781585620050. Retrieved 2009-12-06. "...insomnia is a symptom. It is neither a disease nor a specific condition. (from p. 322)"
^ Morin, Charles M. (2000). "The Nature of Insomnia and the Need to Refine Our Diagnostic Criteria" (Editorial). Psychosomatic Medicine 62 (4): 62:483–485. PMID 10949092. Retrieved 2010-01-07.
Diagnostic and Statistical Manual of Mental DIsorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
National Institutes of Health. National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005. Sleep. 2005;28(9):1049-1057.
International Classification of Sleep Disorders. Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
Sleep Disorders. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text revision. Washington, D.C.; American Psychiatric Association. 2000:551-607.
Kupfer DJ, Foster FG, Reich L, Thompson SK, Weiss B. EEG sleep changes as predictors in depression. Am J Psychiatry. 1976;133(6):622-626.




No comments:
Post a Comment