| Question | Answer | Hint |
| normal pH | pH 7.35-7.45 | |
| most common buffer system | CO2 + H2O — H2CO3 — H+ + HCO3- | |
| normal ratio of carbonic acid to bicarbonate | 1:20 | |
| respiratory acidosis | Increased CO2 results in decrease in pH | |
| respiratory alkalosis | Decreased CO2 results in increase in pH | |
| respiratory component of acid-base balance | CO2 (carbon dioxide) | |
| metabolic acidosis | Increased HCO3 results in increase in pH | |
| metabolic alkalosis | Decreased HCO3 results in decrease in pH | |
| metabolic component of acid-base balance | HCO3 (bicarbonate) | |
| normal PaCO2 | 35-45 mmHg | |
| normal PaO2 | 83-100 mmHg | |
| normal HCO3 | 22-26 mEq/L | |
| ABG analysis step 1 | if pH is <7.35, acidosis if pH is >7.45, alkalosis | |
| ABG analysis step 2 | if CO2 is abnormal, respiratory if HCO3 is abnormal, metabolic | |
| ABG analysis step 3 | pH is normal: fully compensated pH & opposite number out of range: partially compensated pH out of normal range, opposite number in normal range: no compensation | |
| oxyhemoglobin curve | changes in pH alter ease with hemoglobin releases O2 to plasma | |
| values of metabolic acidosis | pH is low, HCO3 is low | |
| values of metabolic alkalosis | pH is high, HCO3 is high | |
| values of respiratory acidosis | pH is low, PaCO2 is high | |
| values of respiratory alkalosis | pH is high, PaCO2 is low | |
| causes of metabolic acidosis | diabetic ketoacidosis, starvation, lactic acidosis, excess ETOH or ASA, renal failure, diarrhea | |
| s/s of metabolic acidosis | lethargy, confusion, stupor, coma, hyporeflexia, muscle weakness, bradycardia, thready pulses, low BP, Kussmaul resp, warm/flushed/dry skin, hyperkalemia | |
| treatment of metabolic acidosis | treat the cause: insulin, hydration/electrolytes, antidiarrheals, sodium bicarbonate, dialysis | |
| causes of metabolic alkalosis | antacid overuse, IV LR overuse, NaHCO3 overuse, vomiting, NG suctioning, thiazide diuretics | |
| s/s of metabolic alkalosis | anxiety, irritability, hyperreflexia, muscle cramps/weakness, tachycardia, normal or low BP, shallow resps, hypokalemia, hypocalcemia | |
| treatment of metabolic alkalosis | treat the cause: fluid/electrolyte replacement, NS IV, Ca++, K-sparing diuretics, antiemetics | |
| causes of respiratory acidosis | head injury, Rx overdose, chest injury, electrolyte imbalance, severe obesity, ascites, hemothorax, COPD, aspiration, pneumonia, pulm edema, TB, PE | |
| s/s of respiratory acidosis | skin pale to cyanotic & dry, increase PaCO2 | |
| treatment of respiratory acidosis | increase CO2 excretion: bronchodilators, steroids, Mucomyst, O2, pulmonary hygiene, PAP | |
| causes of respiratory alkalosis | hyperventilation – anxiety, fear, mechanical ventilation; hypoxemia – asphyxiation, shock, high altitude | |
| s/s of respiratory alkalosis | numbness & tingling around mouth, extremities, resp. effort normal or increase | |
| treatment of respiratory alkalosis | treat underlying condition, support renal function w/ fluids, breath into bag or rebreather, sedatives |
Showing posts with label ABG's. Show all posts
Showing posts with label ABG's. Show all posts
Mar 7, 2015
ABG, Blood Gases, Alkalosis, Acidosis....
Labels:
ABG's,
Acidosis,
Alkalosis,
Blood Gas,
Breathing,
lungs,
Metabolic,
PH,
Respiratory,
Respiratory Assessment
Fluid, Electrolytes, and Acid-Base Balance....
I. Fluid and Electrolytes
- A. Water is the largest single component of the body
- B. 60% of the average adult’s body is fluid
- C. Homeostasis is the ability to maintain internal balance in the presence of external stressors
II. The Purpose of Body Fluids
A. Medium for transportation
- 1. Nutrients to cells
- 2. Wastes from cells
- 3. Hormones, enzymes, blood platelets, RBCs & WBCs
B. Cellular metabolism/chemical functioning
C. Normal body temperature
D. Facilitates digestion & elimination
E. Tissue lubricant
F. Solvent for electrolytes & nonelectrolytes
III. Body Fluids Overview
A. Intracellular ICF within the cells 40% body wtB. Extracellular ECF (20% body wt)
- 1. Intravascular IVF contained within blood vessels
- a. 5% body wt
- 2. Interstitial ISF surrounds cells, includes lymph
- a. 15% body wt
C. Transcellular TCF includes cerebrospinal, pericardial, pleural, synovial and intraocular fluids, sweat, + digestive secretions <1% body wt
IV. Composition of Body Fluids
A. Electrolytes
- 1. Ions
- a. Cations
- 1. Positively charged: sodium, potassium, calcium
- b. Anions
- 1. Negatively charged: chloride, bicarbonate, sulfate
V. Variations in Fluid Content
A. Age
- 1. Infant 77% water
- 2. Adult 60% water
- 3. Elderly 45% water
B. Gender
C. Body Mass
VI. Movement of Body Fluids
A. Osmosis
- 1. movement of a pure solvent through semipermeable membrane from area of low concentration to area of greater concentration
- B. Diffusion
- 1. movement of a solute in solution across a semipermeable membrane from area of high concentration to area of low concentration
C. Filtration
- 1. Process by which water & diffusible substances move together in response to fluid pressure; movement is from higher to lower pressure
D. Active Transport
- 1. Requires metabolic activity & expenditure of energy to move materials across cell membranes
VII. Osmosis
A. A shift of fluid from an area of low concentration to an area of higher concentration until the solutions are of equal concentration.
B. Membrane is permeable to the solvent, not the solute
C. Tonicity is the ability of solutes to cause osmotic driving forces
D. Moses moved water
VIII. Osmotic Pressure
A. Tonicity is the ability of solutes to cause osmotic driving forces
B. Exerted on permeable membranes by high molecular weight substances
C. To pull fluid across membranes
IX. Osmotic Pressure
A. A fluid with a high solute concentration has a high osmotic pressure
B. Of two solutions, higher osmotic pressure will draw fluid until equilibrium is reached
C. Osmotic pressure of a solution is called osmolarity
D. Osmolarity is measure used to evaluate serum and urine in clinical practice
E. Expressed in osmols, or milliosmols per kilogram (mOsm/kg)
F. Normal serum osmolarity is 280-295 mOsm/kg
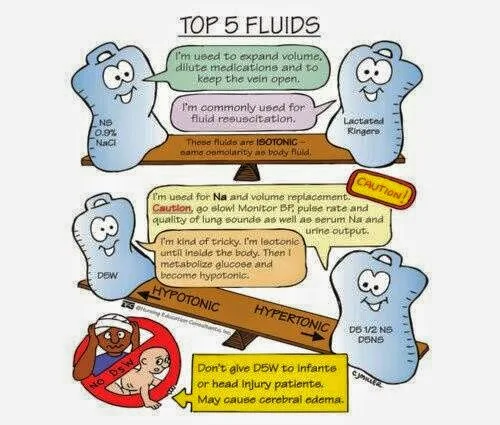
X. Types of Solutions
A. Isotonic – .9%/Normal Saline
- 1. Same concentration of solute as blood
- 2. Expands body’s fluids without causing fluid shift
B. Hypertonic (hyperosmolar) – D5NS, LR
- 1. Greater concentration of solutes than blood
- 2. Pulls fluids from cells causing them to shrink
C. Hypotonic (hypo-osmolar) – .45% NS
- 1. lesser concentration of solutes than blood
- 2. Moves fluid into the cells, causing enlargement
XI. Colloidal Osmotic/Oncotic Pressure
A. Affected by naturally produced serum proteins
B. Albumin exerts colloid pressure to keep fluid in the intravascular compartment by pulling water from the interstitial space back into the capillaries
XII. Diffusion
A. Is the natural tendency of a substance (or gas) to move from an area of higher concentration to one of lower concentration
B. This achieves balance
C. The difference between the two concentrations is called the concentration gradient
XIII. Facilitated Diffusion
A. Diffusion is facilitated by a carrier substance.
B. Facilitated diffusion requires a concentration gradient and sufficient carriers
C. Example: O2 & CO2 exchange
XIV. Filtration
A. Process of water and diffusible substances move together in response to fluid pressure
- 1. Called hydrostatic pressure
- 2. Determines the movement of water
B. Examples
- 1. Increased hydrostatic pressure on the venous side (congestive heart failure) water and electrolytes from the arterial capillary bed move to the interstitial fluid
- 2. Results in edema
A. Is necessary in the absence of concentration gradient or electrochemical gradient
B. Requires metabolic activity, expenditure of energy and, carrier substances to move materials across cell membranes
C. Allows cells to move molecules otherwise immovable – “uphill”
D. Examples
- 1. Na+ & K+ movement against the gradient
- 2. Mechanism that allows cells to absorb glucose & other substances to facilitate metabolic activities
XVI. Body Fluid Regulation
A. Homeostasis – physiological balance
B. Allows body to respond to disturbances in fluid & electrolyte levels to prevent & repair damage
C. Fluid intake
D. Hormonal regulation
E. Fluid output regulation
XVII. Cardiovascular System
A. Maintains:
- 1. Blood pressure
- 2. Cardiac output
- 3. Hydrostatic pressure
- 4. Adequate glomerular filtration rate
XVIII. Definitions
A. Osmolality
- 1. The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per kilogram of solvent
B. Osmolarity
- 1. The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per liter of solution
A. Regulated through the thirst mechanism located in the hypothalamus
B. Conscious desire for water
C. One of the major factors in fluid intake
D. Osmoreceptors monitor serum osmotic pressure; osmolality increases; hypothalamus is stimulated; thirst results
- 1. Increased osmolality – can occur with inability to take in fluids or administration of hypertonic fluids
- 2. Vomiting or hemorrhage: Hypovolemia; dehydration
XX. Hormonal Regulation (Endocrine)
A. Antidiuretic hormone (ADH)
- 1. Stored in posterior pituitary gland
- 2. Released in response to changes in blood osmolarity
B. Aldosterone
- 1. Released by adrenal cortex in response to increased plasma K+ levels or part of renin-angiotensin-aldosterone mechanism in hypovolemia
C. Renin
- 1. Proteolytic enzyme secreted by kidneys, responds to decreased renal perfusion 2nd to decrease extracellular volume
- 2. Triggers angiotensin I production converting to angiotensin II which causes massive selective vasoconstriction ultimately directing blood to perfuse kidneys
XXI. Fluid Output Regulation
A. Occurs through four organs of water loss
- 1. Kidneys
- a. Major regulatory organs of fluid balance; receive 180 L of plasma to filter & produce 1200 to 1500 ml of urine/day
- 2. Skin
- a. Regulated by the sympathetic nervous system; activates sweat glands
- b. Sensible – excess perspiration; can be observed
- c. Insensible – continuous; not perceived by the person; can increase significantly with fever or burns
- 3. Lungs
- a. Expire about 400 ml of water daily
- 4. Gastrointestinal tract (GI)
- a. 3 to 6 L of isotonic fluid moved into GI tract & returned to extracellular fluid daily
XXII. Regulation of Electrolytes
A. Cations
- 1. Sodium
- 2. Potassium
- 3. Calcium
- 4. Magnesium
B. Anions
- 1. Chloride
- 2. Bicarbonate
- 3. Phosphorus-phosphate
XXIII. Fluid Shifts
A. First Spacing
- 1. Normal fluid compartments
B. Second Spacing
- 1. Interstitial
C. Third Spacing
- 1. When fluid is trapped in a body space as a result of injury or disease,
- 2. Represents a fluid loss
- 3. Includes pericardial, pleural, peritoneal, joints
XXIV. Plasma to Interstitial
A. Pathology
- 1. + hydrostatic pressure
- 2. Decreased capillary osmotic pressure
- 3. + cap permeability
- 4. Obstructed lymph drainage
B. Manifestation
- 1. Edema, hypovolemia
C. Interventions
- 1. Fluid replacement
- 2. Monitor for overload
XXV. Interstitial to Plasma
A. Pathology
- 1. Decreased capillary permeability
- 2. Increased capillary osmotic pressure
B. Manifestations
- 1. Hypervolemia
C. Interventions
- 1. If normal, patient excretes fluid
- 2. With disease, must diurese
XXVI. Fluid Volume Deficit (FVD)
A. Thirst with 2% loss
B. Dry mucus membranes with 6% loss
C. Leads to cellular dehydration
D. Weight is best indicator
XXVII. FVD Causes
A. Anything causing loss of blood volume:
- 1. Blood loss
- 2. Polyuria
- 3. GI losses
- 4. Profuse diaphoresis
- 5. Third spacing
- 6. Decreased intake
XXVIII. FVD Manifestations
A. Hypotension
B. Increased pulse, respirations
C. Decreased urinary output, temperature
D. Poor skin turgor
E. Dry mucus membranes
F. Constipation
G. Increased hematocrit, plasma proteins, BUN, urine specific gravity
XXIX. FVD Interventions
A. Correct the underlying cause
B. Replace fluid depending on type lost
XXX. Fluid Volume Excess (FVE)A. Caused by fluid overload
B. Renal failure
C. CHF
D. Cirrhosis
E. Corticosteroids
F. Cushing’s syndrome
XXXI. FVE Manifestations
A. BP up, bounding pulse
B. Distended neck veins
C. Rapid wt gain
D. Peripheral edema
E. Pulmonary edema
F. CVP elevated
G. BUN decreased, hematocrit decreased
H. Plasma proteins decreased
XXXII. FVE Interventions
A. Treat the underlying cause
B. Fluid and or sodium restriction
C. Diuretics
D. Dialysis, paracentesis
XXXIII. Regulation of Acid-Base Balance
A. Metabolic processes maintain a steady balance between acids & bases
B. Arterial pH inversely proportioned to the hydrogen ion concentration
C. The greater the concentration, the more acidic the solution, the lower the pH & vice versa
D. The lower the concentration, the more alkaline the solution, the higher the pH
XXXIV. Chemical Regulation
A. Largest chemical buffer is carbonic acid & bicarbonate buffer system
B. Carbonic acid – carbon dioxide
C. Bicarbonate – excretion by the kidneys
XXXV. Biological Regulation
A. Occurs when hydrogen ions are absorbed or released by cells
B. Occurs after chemical buffering & takes 2 to 4 hours
C. Hydrogen must exchange with another positively charged ion
- 1. Chloride shift
- 2. Hemoglobin-oxyhemoglobin system
XXXVI. Physiological Regulation
A. Act as buffers (compensation) to return the pH to normal
B. Lungs
- 1. When the respiratory system is the problem agent – resp. acidosis; resp. alkalosis
- 2. Acts as the buffer when renal system is the problem
C. Kidneys
- 1. When the renal system is the problem agent – metabolic acidosis; metabolic alkalosis
- 2. Acts as the buffer when respiratory system is the problem
XXXVII. Disturbances in Electrolyte, Fluid, & Acid-Base Balance
A. Seldom occur alone
B. Can disrupt normal body processes
C. Each disturbance can cascade into a disturbance of the other
XXXVIII. Electrolyte Imbalances
A. Sodium
B. Potassium
C. Calcium
D. Magnesium
E. Chloride
XXXIX. Sodium
A. Hyponatremia
1. Net sodium loss or excess water excess2. Indicators & treatments depend on cause & ECF status
B. Hypernatremia
- 1. Excess water loss or sodium excess
- 2. Increases aldosterone secretion, sodium is retained, potassium is excreted
- 3. Body conserves fluid through renal reabsoption
XXL. Potassium
A. Normal amount is very small with little tolerance for fluctuation
B. Hypokalemia
- 1. One of most common electrolyte imbalances
- 2. Inadequate amount of potassium circulates in the ECF
- 3. Severe cases can affect cardiac conduction and function; most common cause is use of potassium-wasting diuretics
C. Hyperkalemia
- 1. Produces marked cardiac conduction abnormalities
- 2. Primary cause is renal failure; also seen in crushing injuries
Calcium
A. Hypocalcemia
- 1. Results from severe illnesses, especially ones that directly affect thyroid & parathyroid glands; renal insufficiency (inability to excrete phosphorous, as phosphorous rises, calcium declines)
- 2. S/S related to neuromuscular, cardiac, & renal systems
B. Hypercalcemia
- 1. Frequently a symptom of underlying disease resulting in excess bone reabsorption
Magnesium
A. Symptoms are a result of changes in neuromuscular excitability
B. Hypomagnasemia
- 1. Occurs with malnutrition, malabsorption disorders, & neuromuscular system disorders
C. Hypermagnasemia
- 1. Depresses skeletal muscles & nerve function
- 2. Depresses acetylcholine leads to sedative effect; leading to bradycardia, ECG changes, cardiac arrhythmias, decreased respiratory rate & depth
Chloride
A. Commonly associated with acid-base imbalance
B. Hypocloremia
- 1. Occurs with vomiting or prolonged NG tube or fistula drainage with loss of hydrochloric acid
- 2. Use of loop & thiazide diuretics
- 3. Can result in metabolic alkalosis
C. Hypercloremia
- 1. Occurs when serum bicarbonate falls or sodium level rises
Fluid Disturbances
A. Isotonic
- 1. Occur when water & electrolytes are gained or lost in equal proportions
B. Osmolar
- 1. Occur with losses or excesses of only water so that concentration of serum is affected
Acid-Base Balance
A. Arterial blood gases (ABG) are the best way to evaluate
B. Involves analysis of 6 components
- 1. pH
- 2. PaCO2
- 3. PaO2
- 4. Oxygen saturation
- 5. Base excess
- 6. Bicarbonate (HCO3)
C. Deviation from a normal value indicates imbalanc
PH
A. Measures hydrogen ion concentration in body fluids
B. Even slight changes can be potentially life threatening
C. Normal ranges 7.35 to 7.45
D. RULER OF THE BODY
PaCO2
A. Partial pressure of carbon dioxide
B. Reflects depth of pulmonary ventilation
C. Normal range 35 to 45 mm Hg
D. Indicates the concentration of CO2 in the blood
PaO2
A. Partial pressure of oxygen
B. No primary role in acid-base balance regulation if within normal limits
C. Lower levels < 60mm Hg can lead to anaerobic metabolism, resulting in lactic acid production & metabolic acidosis
D. Normal range is 80-100 mm Hg
Oxygen Saturation
A. Point at which hemoglobin is saturated by O2
B. Can be affected by changes in temparture, pH, & PaCO2
C. Normal range is 95% to 99%
Base Excess
A. Amount of blood buffer that exists
B. High value indicates alkalosis
- 1. Can result from sodium bicarbonate, citrate excess with blood transfusions, IV infusions of sodium bicarbonate to correct ketoacidosis
C. Low value indicates acidosis
- 1. Can result from elimination of too many bicarbonate ions, i.e. diarrhea
Bicarbonate (HCO3)
A. Major renal component of acid-base balance
B. Excreted & reproduced by the kidneys to maintain normal acid-base environment
C. Normal range is 22 to 26 mEq/L (this may vary slightly from lab to lab)
D. Indicator of metabolic cause of acidosis or alkalosis
E. Is buffer agent in respiratory acidosis or alkalosis
Types of Acid-Base Imbalances
A. Respiratory Acidosis
- 1. Excessive carbonic acid & increased hydrogen ion concentration (low pH)
B. Respiratory Alkalosis
- 1. Decreased carbonic acid & decreased hydrogen ion concentration (high pH)
C. Metabolic Acidosis
- 1. High acid content in blood causing loss of HCO3
- 2. Analysis of serum electrolytes to detect anoin gap (which reflects unmeasurable anoins)
D. Metabolic Alkalosis
- 1. Heavy loss of acid or increased HCO3 content in blood
- 2. Most common cause is gastric suction
Nursing Knowledge
A. Imbalances can occur at any age
B. Body’s adaptive compensatory mechanisms fail to maintain balance adequately
C. Health becomes compromised
D. Severity & long-term effects can influence client’s ability to return to optimal health
E. Prolonged compromise can lead to irreversible chronic health problems that affect the quality of life for client & family
Nursing Process – Assessment
A. Nursing history
- 1. Client’s history determines goals
- 2. Age of client is important factor
B. Prior medical history
- 1. Acute illnesses
- a. Surgeries, burns, respiratory disorders, head injuries
- 2. Chronic illnesses
- a. Cancer, cardiovascular disease, renal disease, GI disturbances
- 3. Environmental factors
- a. Exercise, exposure to temperature extremes
- 4. Diet
- a. Intake of fluids, changes in appetite, metabolic interference, physical problems
- 5. Lifestyle
- a. Smoking, alcohol use/abuse, drugs
- 6. Medication
- a. Prescription or OTC meds that perpetuate fluid imbalances
Physical Assessment
A. F&E/A-B imbalances can affect all systems
B. Thorough exam
C. Include client’s intake/output history, genitourinary patterns/changes
D. Lab study results
E. Client expectations
Nursing Process – Nursing Diagnoses
A. Actual
- 1. Ineffective breathing patterns
- 2. Decreased cardiac output
- 3. Deficient fluid volume
- 4. Excess fluid volume
- 5. Impaired gas exchange
- 6. Impaired mobility
- 7. Impaired tissue integrity/perfusion
B. Risks
- 1. Imbalanced body temperature
- 2. Deficient fluid volume
- 3. Impaired skin integrity/perfusion
Nursing Process – Planning
A. Goal & Outcomes
- 1. Client free of complication
- 2. Demonstrates fluid balance
- 3. Labs in range
B. Setting Priorities
- 1. Client’s condition sets priorities of ND
C. Continuity of Care
- y1. Discharge planning should happen early
Nursing Process – Implementation
A. Health promotion
- 1. Teach client & family to recognize risk factors
- a. Age, activities, specific chronic illness affects
B. Acute care
- 1. Daily weights
- 2. Enteral replacement of fluids
- 3. Fluid restrictions
- 4. Parenteral fluid & electrolyte replacement
- 5. IV therapy implications & risks
Complications of IV Fluid Administration
A. Systemic:
- 1. Fluid Overload
- 2. Air Embolism
- 3. Septicemia
B. Local:
- 1. Infiltration and Extravasation
- 2. Phlebitis
- 3. Thrombophlebitis
- 4. Hematoma
- 5. Clotting and obstructing
Fluid Overload
A. Fluid Overload: too much fluid in circulatory system: Rapid infusion, underlying cardiac, liver, or renal disease
B. S+S: moist crackles, edema, wt gain, dyspnea, shallow rapid resp
C. Treatment: Decrease flow rate, monitor VS + BS, position High Fowlers
D. Prevent: IV pumps, careful assessment
E. Complications: CHF, Pulmonary edema
Air Embolism
A. Occurs when air enters the bloodstream.
B. Is threatening when the air displaces blood to the cells
C. Most often associated with central veins
D. S+S; dyspnea, cyanosis, hypotension, weak, rapid pulse, loss of consciousness, chest shoulder, low back pain. Complication: death
E. Treatment
- 1. Clamp iv lines;
- 2. L trendelenberg position;
F. Prevention
- 1. Careful filling of IV tubes and syringes;
- 2. LuerLock adapters;
- 3. Air sensing pumps
Septicemia
A. Infection disseminated through the blood stream
B. Cause:
- 1. Contaminated IV products, break in technique
C. Risk: immunocompromised
D. S+S:
- 1. Elevated Temp, backache, headache, pulse and resp elev.
E. Treatment:
- 1. Symptomatic, local or systemic
F. Prevention:
- 1. Critical hygiene and technique
Infiltration
A. Infiltration:
- 1. Introduction of a non vesicant solution into surrounding tissues
- 2. Extravasation: Introduction of a vesicant or irritating solution into surrounding tissues.
B. S+S: edema, coolness, decreased flow, discomfort
C. Tx:
- 1. Discontinue, restart, compress with warm or cold to affected site, elevate
D. Prevention:
- 1. Careful securing of IV tubing, limit mobility of limb with IV, frequent observation of site
Phlebitis & Thrombophlebitis
A. Phlebitis:
- 1. inflammation of a vein from chemical or mechanical irritation.
- 2. S+S: red, warm at site or along vein, pain, tenderness, swelling.
- 3. Prevention: (frequency parallels length of insertion), use good aseptic technique, observe frequently.
- 4. Tx: discontinue IV, warm moist compress, elevate
B. Thrombophlebitis:
- 1. presence of a clot in addition to phlebitis.
- 2. S+S: same + more discomfort, elevated WBC, immobility
- 3. Tx: same: Prevent: avoid trauma at insert.
Hematoma
A. Blood leaking into tissue.
B. From perforation of vein during insertion or later.
C. S+S: ecchymosis, swelling, leak blood
D. Tx: remove, pressure, +/- ice, heat.
E. Prevent: careful technique during insertion
Clotting and Obstruction
A. Occur from kinked tubing, slow infusion rate, failure to flush line, empty IV bag
B. S+S: decreased flow, blood backing up,
C. Tx: if clotted, restarting at a new site is necessary
Nursing Process – Evaluation
A. Client care
- 1. Client teaching
- 2. Recognition of signs/symptoms of imbalance
- 3. Consult physician to enhance care in chronic conditions
B. Client expectations
- 1. Evaluate the client’s perception of care and goals
- 2. Use client input to understand needs and expectations
Labels:
ABG's,
Acidosis,
Alkalosis,
Breathing,
Fluid and Electrolytes,
Fluid Balance,
Fluids,
Hydration,
Metabolic,
Respiratory Assessment
Cardiac System Oxygenation Help....
Cardio – Oxygen Questions Study Guide
| Question | Answer | Hint |
| Normal functioning of the lungs depends on what three factors? | patent respiratory tree, functioning alveoli system, well functioning cardiovascular system | |
| What is meant by a patent respiratory tree? | open, able to move air. If there is an occlusion or obstruction it is not patent and will have a negative impact on the respiratory sys. | |
| What is the main function of the upper airway? | warms air, humidifies, filters air, and helps get microorganisms out | |
| What are cilia and what are their main function? | hair like projections in the airway that help get contaminants out of the respiratory tree. | |
| What are the functions of mucus and coughing? | Mucus helps to capture microbs while coughing helps move secretions out. | |
| What helps to thin mucus in the lungs? | Hydration | |
| What is the function of surfactant? | helps to keep the alveoli open/inflated and decreases surface tension | |
| What is ventilation? | the movement of air in and out of the lungs | |
| define/describe inhalation | active process, muscles contract, diaphragm moves down, pressure goes down and air rushes in | |
| define/describe exhalation | passive process, muscles relax, diaphragm moves up, pressure goes up and air rushes out | |
| What are 3 factors that affect respiration? | Accessory muscles, lung compiance, and airway resistance | |
| What are the accessory muscles and what do they do? | They are the abdominal, intercostal, and sternocleidomastoid muscles which help the distressed pt. move air | |
| What is lung compliance? | elasticity of lungs to expand; how easily the lungs expand. Decreased lung compliance means decreased elasticity | |
| What factors affect lung compliance? | chest wall factors (position of the body-MS, obesity, lying in bed, etc.) and lung factors (problems in the lungs- pneumonia, fibrosis, pulmnary edema, etc.) | |
| What is atelectasis? | decreased expansion of the lungs | |
| What is pleural effusion? | collection of fluid between lung and chest wall. Fluid collapses the lungs. | |
| What is pulmonary edema? | fluid inside the respiratory tree such as with lf. side heart failure- blood gets backed up into the lungs and dumped into the alveoli because heart can’t pump it out properly. | |
| What is pulmonary fibrosis or pulmonary htn? | after an injury occurs fibrin and collagen are laid down to repair which toughens lung tissue and decreasing compliance | |
| What is pneumothorax? | a collapse of a portion of lung with air in the pleural space | |
| What is hemothorax? | blood in the pleural space | |
| What can cause airway resistance? | any obstructions to airflow: narrowed tube, tumor, infection, secretions, edema, foreign objects, bronchial constriciton, etc. | |
| define diffusion | movement of SOLUTES from an area of greater concentration to an area of lesser concentration | |
| define osmosis | movement of SOLVENT from and area of lesser concentration to an area of greater concentration | |
| define perfusion | movement of fluid (blood) through or into a system (blood entering vessels through walls) | |
| Diffusion and perfusion are interrelated, therefore can you have one without the other? | Yes, it is possible to have diffusion but not perfusion however diffusion will not be effective. For example air is moving into the lungs, but there is a blocked area of tissue so perfusion is not happening | |
| What things effect diffusion in the lungs? | surface area (less area = less diffusion), disease, and a decrease in environmental O2 | |
| What types of things can affect the amount of surface area in the lungs? | body position, tumor, lung collapse, lung removal, muscus plug, immobility, etc. | |
| How is oxygen transported through the body? | 97% is attached and transported via hemoglobin and 3% is dissolved into plasma | |
| The amount of oxygen that binds to hgb depends on what? | PaO2 : more PaO2 the more oxygen that attached to Hgb | |
| What is a normal PaO2? | between 80-100mmhg | |
| At a PaO2 of 60mmhg how saturated are the Hbg with oxygen (SaO2)? | 90% | |
| What is hypoxemia? | decreased O2 in blood and causes hypoxia | |
| What is hypoxia? | decreased O2 in the tissues | |
| What are some sx/s of hypoxia? | cyanosis, pale coloration of skin, apprehensive, restless, confused, c/o dyspnea | |
| What controls respirations in a healthy person? | CO2: CO2 crosses the bbb and mixes with H2O. H+ ions increase which causes faster breathing. | |
| What controls respriation in a nonhealthy person? | O2 : since a nonhealthy person lives with high levels of CO2 because of the build up, O2 must therefor control the respiratory drive. Low levels of O2 increases breathing | |
| Why is it important to monitor a pt. with COPD who is on oxygen? | Because if the O2 levels get too high then their respriatory drive is not triggered and the pt. can stop breathing | |
| What are two ways of measuring O2 in the blood? | ABG (arterial blood gas) and Pulse oximeter (saturation of O2) | |
| What are the normal ranges of PaO2 and PaCO2? | PaO2:80-100mmhg PaCO2:35-45mmhg | |
| What does and ABG tell us? | How well diffusion is functioning in the lungs | |
| What would a venus draw(VBG) tell us? | how much O2 is being used by the tissues; tells us the O2 demand in the peripheries | |
| True or false?ABG will help us make critical decisions and tells us if the pt. needs O2 therapy. | True | |
| What is a normal level on a pulse ox? | 95-100% but anything over 90% is good | |
| True or false? pulse ox will help us make critical decisions and tells us if the pt. needs O2 therapy. | False. It does not help make critical decisions, but may determine if a ABG is needed | |
| How can a pulse ox give a misreading of O2 saturation? | If Hgb is low but still 90% saturated it could read 90%SaO2 when the pt. is actually hypoxic or hypoxemic because of the low Hbg levels | |
| What types of pts need O2 therapy? | if they are hypoxic or hypoxemic, someone with a non-respiratory problem and demands more O2 to the tissues such as a febrile pt, someone with low levels of Hgb such as with blood loss or burn victims, someone with reduced O2 carrying ability such as a post-op pt, someone with decreased cardiac output | |
| What is the % of O2 (fraction of inspired air FiO2) in room air? | 21% | |
| True or false? If over 2L/min of O2 is delivered then it needs to be humidified. | True | |
| True or false? you need a dr. order to humidify but not to administer O2. | False. Oxygen is considered a drug and you need a dr.s order for it however you do not need an order to humidify | |
| Up to how many L of O2 can be given with nasal prongs? | 6L/min | |
| simple face mask | delivers 5-8L/min O2, 40-60% FiO2, fits snugly, has vents to pull in room air and expel CO2 | |
| Partial rebreather | has reservoir bag and vents, needs humidity, delivers 5-11 L/min O2, 60-75% FiO2, | |
| Non-rebreather | same as partial rebreather except it has vents, prevents outside air and exhaled CO2 from mixing with O2, needs to be monitored, delivers 6-15 L/min O2, 80-90% FiO2 | |
| Venti mask | only delivers up to 50% FiO2 but is more accurate than other masks because you can control the amount of O2 and room air that is given | |
| What are 5 precautions when using oxygen? |
|
Labels:
ABG's,
Airway Assessment,
Breathing,
lungs,
Oxygen,
Pneumothorax,
Pulmonary,
Respiratory Assessment,
Respiratory System
Subscribe to:
Comments (Atom)